Remember, I am not a doctor, nor do I play one on Substack. Keep advocating for yourselves, and please see your doctor with medical questions. Also, I’m not a reporter; I'm someone sharing her experience.
You all had a lot to say about last week’s post.
Remember we talked about why I’m not getting mammograms anymore? I heard from several of you who have experienced breast cancer, and you told me how early detection helped save your life.
So that’s what we’re talking about this week—early detection.
Thanks to each of you who took the time to comment, email, or message me to share your stories and personal experiences. I learned a lot, and I hope to convey some of it here today.
Early detection is important, here’s why:
Breast cancer is the second most diagnosed cancer in women (skin cancer is first).
One in eight women will be diagnosed with breast cancer in the US.
Early detection (meaning you find it before symptoms begin - a lump is a symptom) has a 93 percent higher survival rate in the first five years.
There has been a rapid rise in breast cancer found in women under 50.
So, how do you detect it early?
Basically two ways:
Regular screenings (mammogram, ultrasound, MRI, etc.)
Breast exams (both by your doctor and yourself) well, maybe. I’ll talk about this later.
Screenings are where it’s at.
You’re busy. I get that. These are the things that are easy to ‘push off’ until a more convenient time, but let’s be honest, there will never be a more convenient time. You know this; I know this. It’s important to schedule your screening as soon as you can.
Now, let’s get to it.
Here is what I’ve learned from you (and a little from Dr. Google).
Screening recommendations are based on risk:
Your doctor will recommend screening based on your individual risk factors. (You can assess your risk using this tool. )
I pulled this from the CDC website:
The US Preventive Services Task Force is an organization made up of doctors and disease experts who look at research on the best way to prevent diseases and make recommendations on how doctors can help patients avoid diseases or find them early.
The Task Force recommends that women who are 40 to 74 years old and are at average risk for breast cancer get a mammogram every 2 years. Women should weigh the benefits and risks of screening tests (see below). Different screening recommendations may be used for women at higher than average risk.
This is blowing my mind a little bit.
Because here’s what you, my readers, are telling me:
These are stories from women I know. Granted, the sample size is a handful, so keep that in mind, but still. I’ve changed their names, but I kept the stories intact. Read on.
Ann had not missed an annual mammogram and had no family history of breast cancer - this means she would be of average risk. She went from a clear mammogram to stage 2 cancer within the year.
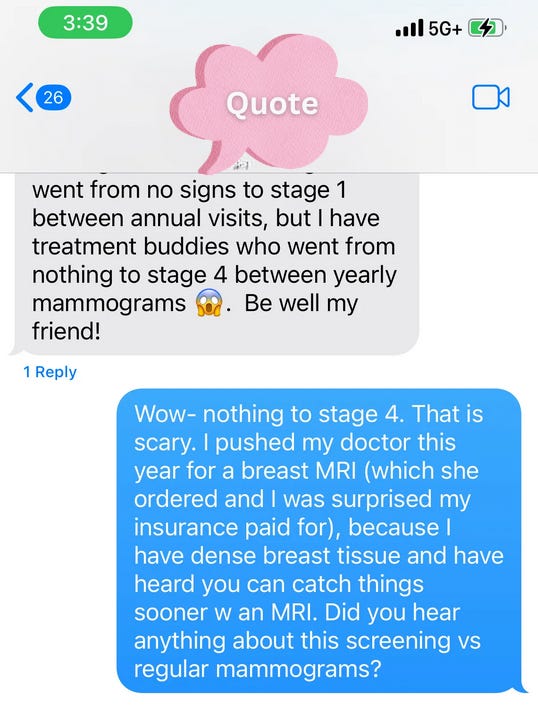
Stacy also gets annual screenings, and when she was diagnosed, she was stage 1. Some of the women she was in treatment with, however, weren’t so lucky and told stories of how they went from a clean mammogram to stage 4 between annual screenings.
Stacy and Ann benefited from early detection and are on the other side of treatment. Stacy has less than a 3% chance of recurrence. I hope that’s the case for Ann, but that’s not something she discussed with me.
Even though the CDC recommends a screening every other year, most hospitals and breast clinics still recommend one annually. The American Cancer Society recommends switching to every other year at age 55.
Breast exams and breast self-awareness:
From what I’ve read, it’s more important to be familiar with your breasts than to do a monthly check. If you’re familiar with what’s normal, it will be easier to detect if something changes. Remember, a lump is a symptom, so while it’s wise to check for changes in your breast tissue, screening is the best way to detect breast cancer before symptoms occur.
Ask your doctor to show you what’s normal at your next clinical exam.
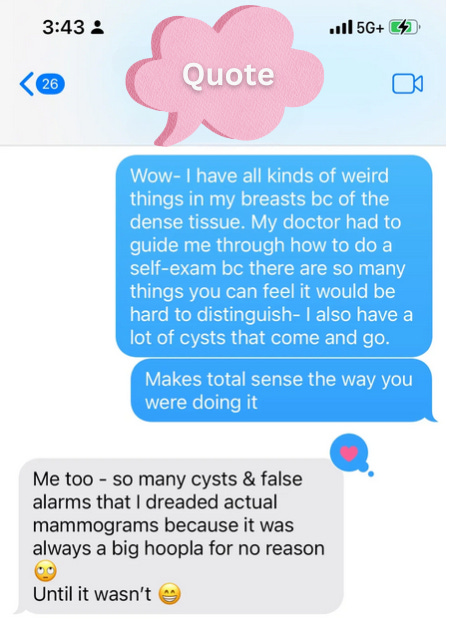
In addition to having dense breast tissue, I’m also prone to cysts, which feel like little lumps (because they are). There is so much ‘gunk’ in there when I do my self-checks.
In my 20s, I asked my doctor to take me through each breast and to show me what was normal and what to look for when something wasn’t normal. I do my best, but I know it isn’t a perfect self-check, which may not matter much because…
Here’s something that surprised me from the CDC:
Do you know what has? Screening.
Check the whole breast:
Be sure to check the entire breast. Ann had a lump right beneath the nipple and never felt it because she began her monthly checks around the nipple, not on it. Also, be sure to check the area around the outside of the breast and under the armpit.
Stacy told me she never felt the lump, even when the doctor tried to show her during her clinical breast exams.
Ann also reminded me that as someone with a history of breast cancer, she must suppress her hormones and cannot take HRT (which I wrote about here).
At what age should you begin (and stop) screenings?
The CDC recommends women aged 40 to 74.
But maybe that’s not always the case. As I mentioned above, there is an increase in occurrences of breast cancer in younger women.
Someone else wrote to me to say her sister-in-law was diagnosed when she was 88.
What about the risk?
I could tell from your comments that some of you are concerned about the amount of radiation in a mammogram. I did some digging. Do you know there is radiation all around us? The radiation in a typical mammogram equals about two months of the radiation you get just by walking around. Or about 4,000 bananas.
There’s hope if you get a diagnosis:
Ann told me: “There are many options for treatment - it seems as if the research has really taken off.” Indeed, the treatment options have never been greater, especially if you detect it early.
And remember, if you are diagnosed, you might want to consider getting a second opinion from someone at a major cancer center- the protocol they recommend for treatment can be administered anywhere - like in your hometown.
And one last thing:
I learned that the standard of care for someone higher on the risk scale is to screen with both an MRI and a mammogram, so I’ll ask my doctor about that.
Thanks for growing with me in this. Let’s keep learning from each other and advocating for ourselves.
LYLAS -
S
PS - Besides what’s linked here, I also read this, this ,this, and this.
I would love to get another conversation started if you feel comfortable sharing. If not, I hope you were able to glean some healthy knowledge you might not have known.






This was such a good read, especially the quotes from your readers. It's scary to know it can progress so quickly in some women.
My grandma was diagnosed in her 80s and had a mastectomy at 82!! I thought that felt rather late in life for breast cancer. Thankfully she was a tough old lady and lived til 94 😊
Great post, Sara!
Nice